Nobel Prize in Medicine Winners 2025 Out: How Three Scientists Discovered the Immune System's Security Guards and Why It Matters
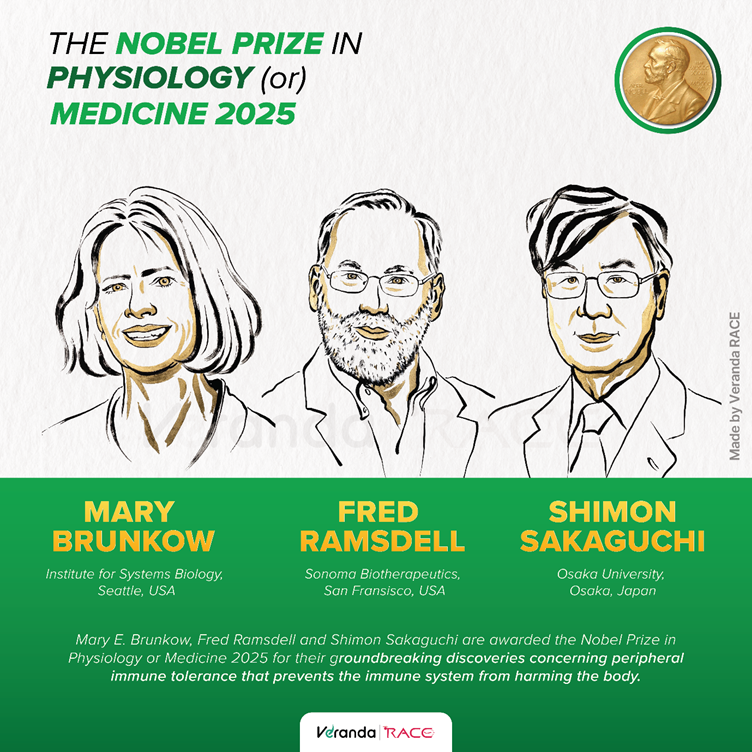
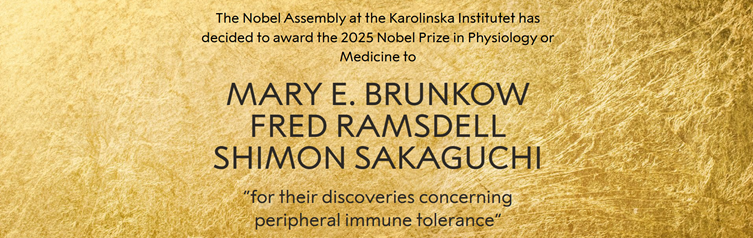
The Nobel Prize in Physiology or Medicine 2025 has been awarded to Mary Brunkow, Fred Ramsdell and Shimon Sakaguchi “for their discoveries concerning peripheral immune tolerance” by the Nobel Assembly at the Karolinska Institutet in Sweden.
Among this year’s Medicine Nobel winners in 2025, Mary Brunkow and Fred Ramsdell are from the United States, while Shimon Sakaguchi is from Japan.The trio will now share the prize money of 11 million Swedish kronor (nearly $1.2 million).
Their discoveries have fundamentally changed our understanding of how the human immune system protects us without attacking our own bodies. Their work on regulatory T cells and peripheral immune tolerance has opened new pathways for treating cancer, autoimmune diseases and organ transplant rejection.
But what exactly did these scientists discover to have been awarded as the Nobel Prize in Physiology or Medicine Winners in 20225 and why does it matter to ordinary people? Let's break it down.
The Fundamental Problem
The human immune system is remarkably powerful and complex. Every single day, your immune system fights off thousands of bacteria, viruses and other microbes trying to invade your body. Without it, you wouldn't survive even a week.
But here's the puzzle that has fascinated scientists for decades: How does the immune system know what to attack and what to leave alone? Many disease-causing microbes have evolved to look remarkably similar to our own healthy cells, like wearing camouflage. Some cancer cells hide by mimicking normal tissue. Yet somehow, most of the time, our immune system gets it right.
When it gets it wrong, the consequences are serious. Some autoimmune diseases occur when the immune system mistakenly attacks the body's own tissues. Understanding this delicate balance is crucial for treating these conditions and for helping transplanted organs survive in new bodies.
What are T cells and what is their job?
To understand this year's Nobel Prize in Medicine 2025 winners’ groundbreaking discovery, you need to know about T cells, the frontline soldiers of your immune system.
Helper T cells constantly patrol your body like security guards walking through a building. When they spot an invading virus or bacteria, they sound the alarm and call in reinforcements.
Killer T cells are the special forces. They destroy cells that have been infected by viruses or have turned cancerous.
Both types of T cells have special proteins on their surface called T-cell receptors. Think of these as sensors that can scan other cells to check if everything is normal or if there's a threat. The human body can theoretically produce more than a million trillion different T-cell receptors, ensuring that there's always one that can recognise a new invader, even novel viruses like the one that caused COVID-19.
But here's the problem: among this vast array of T cells, some inevitably develop receptors that recognise our own healthy tissue as a threat. So, what stops them from attacking?
The Thymus
For decades, scientists believed they had the answer. They knew about an organ called the thymus, located just behind your sternum. The thymus is particularly active in babies and children and this is where T cells mature.
Researchers discovered that the thymus performs a crucial test. As T cells pass through, those that react to the body's own tissues are eliminated before they can enter the bloodstream. This process was called "central tolerance" because it happens in a central organ.
This seemed like a complete explanation. But it wasn't.
Shimon Sakaguchi's revolutionary insight
In the 1990s, Japanese scientist Shimon Sakaguchi was working at the Aichi Cancer Centre Research Institute in Nagoya when he noticed something odd. His colleagues had been removing the thymus from newborn mice to study its role in immune development. They expected these mice to have weaker immune systems.
Instead, if the thymus was removed three days after birth, the opposite happened. The mice's immune systems went into overdrive, attacking their own bodies and causing various autoimmune diseases.
This didn't make sense according to the prevailing theory. Sakaguchi became convinced that there must be another mechanism at work, something beyond the thymus's quality control. He suspected the existence of specialised T cells that actively calm down other T cells and prevent them from attacking the body.
In a series of carefully designed experiments throughout the 1980s and early 1990s, Sakaguchi isolated mature T cells from healthy mice and injected them into mice without a thymus. The result was striking: the healthy T cells protected the mice from developing autoimmune diseases.
In 1995, Shimon Sakaguchi published his landmark discovery. He had identified a completely new class of T cells that carry two proteins on their surface: CD4 (found on helper T cells) and CD25 (a marker that distinguished these special cells). He called them regulatory T cells.
These cells don't attack invaders. Instead, they patrol the immune system itself, telling overly aggressive T cells to stand down. They're like security guards watching over other security guards.
The Scepticism
Shimon Sakaguchi's discovery of regulatory T cells faced intense scepticism. In the 1970s and early 1980s, some researchers had claimed to find "suppressor T cells" that controlled immune responses, but many of those studies turned out to be flawed or even fraudulent. The entire concept had been discredited and scientists were reluctant to believe in any similar idea.
Sakaguchi needed more proof. That proof would come from two American researchers working on an entirely different problem, thousands of miles away.
Enter Mary Brunkow and Fred Ramsdell
In the 1940s, at a laboratory in Oak Ridge, Tennessee, researchers studying the effects of radiation noticed something unusual. Some male mice were being born with scaly skin, enormously enlarged spleens and such severe health problems that they died within weeks. The researchers named this strain ‘scurfy’ mice.
By the 1990s, scientists understood that these mice suffered from an autoimmune disease caused by a mutation on the X chromosome. Their immune systems were attacking their own organs. But which gene was responsible?
Mary Brunkow and Fred Ramsdell, working at a biotech company in Washington, USA, decided to find out. They were developing treatments for autoimmune diseases and realised that understanding the scurfy mutation could provide crucial insights.
Finding a single mutated gene among the 170 million base pairs of the mouse X chromosome was like searching for a needle in a haystack. It took years of painstaking work. They narrowed down the search area to 500,000 nucleotides, then identified 20 potential genes in that region. Gene by gene, they compared healthy mice to scurfy mice.
Only with the twentieth and final gene did they find their answer. They had discovered a previously unknown gene, which they named FOXP3 (part of the "forkhead box" gene family).
The Human Connection
While conducting their research, Brunkow and Ramsdell began to suspect that a rare and devastating human disease might be related to what they were seeing in mice. IPEX (Immune dysregulation, Polyendocrinopathy, Enteropathy, X-linked) is a condition that affects young boys, causing severe autoimmune problems. Like the scurfy mutation, it's linked to the X chromosome.
They found the human equivalent of the FOXP3 gene and collected samples from boys with IPEX around the world. Their hunch was correct: mutations in the human FOXP3 gene caused IPEX.
In 2001, Brunkow and Ramsdell published their findings in Nature Genetics. They had discovered that the same gene caused disease in both mice and humans.
The pieces come together: FOXP3 controls regulatory T cells
This is where the two stories merged beautifully. Within two years, Shimon Sakaguchi and other researchers proved the connection: the FOXP3 gene controls the development of regulatory T cells.
Without functioning FOXP3, the body can't produce enough regulatory T cells. Without regulatory T cells, the immune system has no brakes. It attacks everything in sight, including the body's own organs.
The three scientists had, through separate paths of research, uncovered a fundamental mechanism that scientists now call ‘peripheral immune tolerance’. Unlike central tolerance (which happens in the thymus), peripheral tolerance happens throughout the body, with regulatory T cells constantly monitoring and controlling immune responses.
Why this matters?
The discovery of regulatory T cells has launched an entirely new field of medical research with profound implications for treating disease.
For cancer treatment: Tumours are often surrounded by large numbers of regulatory T cells that protect them from immune attack. Cancer researchers are now investigating how to temporarily reduce regulatory T cell activity around tumours, allowing the immune system to recognise and destroy cancer cells. This could lead to more effective immunotherapy treatments.
For autoimmune diseases: The opposite strategy applies here. Researchers are testing ways to boost regulatory T cell numbers in patients with conditions like rheumatoid arthritis, inflammatory bowel disease and Type 1 diabetes. Early clinical trials are using interleukin-2, a substance that helps regulatory T cells thrive and multiply.
For organ transplants: When someone receives a transplanted organ, their immune system sees it as foreign and tries to reject it. Patients must take powerful immunosuppressive drugs for life. Researchers are now exploring whether they can isolate a patient's regulatory T cells, multiply them in the laboratory and return them to the patient's body where they can specifically protect the transplanted organ without suppressing the entire immune system.
Nobel Prize in Medicine Winners of 2025
Mary E Brunkow, born in 1961, currently works at the Institute for Systems Biology in Seattle, United States. Her patient, methodical approach to genetic research was crucial in identifying the FOXP3 gene.
Fred Ramsdell, born in 1960, now serves as Scientific Advisor at Sonoma Biotherapeutics in San Francisco, United States. His collaboration with Brunkow and his insights into autoimmune diseases helped connect the dots between mouse and human disease.
Shimon Sakaguchi, born in 1951, is a Distinguished Professor at the Immunology Frontier Research Centre at Osaka University, Japan. His willingness to challenge scientific consensus and pursue an unpopular hypothesis eventually revolutionised immunology.
Nobel Prize in Physiology or Medicine: Quick Facts
The Nobel Prize in Physiology or Medicine is awarded by the Nobel Assembly at the Karolinska Institutet in Stockholm, Sweden for outstanding discoveries in physiology or medicine.
As of 2024, 116 Nobel Prizes in Physiology or Medicine have been awarded since 1901. It was not awarded in nine occasions: 1915, 1916, 1917, 1918, 1921, 1925, 1940, 1941 and 1942.
232 individuals have been awarded the Nobel Prize in Physiology or Medicine from 1901 to 2025.
The youngest Nobel laureate in Medicine is Frederick Banting (31 years) for the discovery of insulin in 1923.
The oldest Nobel laureate in Medicine is Peyton Rous (87 years) for his discovery of tumour inducing viruses in 1966.
FAQs
Veranda RACE’s Bank Triumphants
IBPS Clerk Exam 2024
My parents suggested me to join Veranda RACE and prepare for Bank Exams. Within 8 months, I've achieved a Bank job in Central Bank of India. I used to attend tests in the computer lab at my offline branch for more than 6 hours. My mentors cleared all my doubts and my faculty motivated me and taught focus strategies to clear the IBPS Clerk Exam.
Jebakumar
IBPS Clerk Exam 2024

SBI PO Exam 2024
Thanks to Veranda RACE, I've cracked three Bank Exams - IBPS PO, SBI PO and IBPS Clerk. Coming a village in Tuticorin, Veranda RACE faculty helped me understand the syllabus and topics of Bank Exams. With full focus on Bank exams, I used to prepare daily in the computer lab and library with constant support from my Bank mentors. They cleared all my doubts without any hesitation.
Thanga Vignesh
SBI PO Exam 2024

AIC MT Exam 2024
I prepared for Bank Exams in Veranda RACE’s Tambaram branch. They trained me specifically for the ‘Agriculture Insurance Company’ Exam. I’m happy that I could contribute more to the profession of my choice! Thanks to the faculty and mentors of Veranda RACE!
Amsalekha
Management Trainee, AIC

LIC ADO Exam 2024
Preparing from Tirunelveli, I want to thank my faculty for the constant support and motivation to crack the LIC ADO Exam. The lab facilities were top notch and I used to prepare writing online mock tests at the computer lab. This was the major reason for cracking the exam in the first attempt. Thanks, Veranda RACE!
Hariharasudhan
Junior Clerk-cum-TypistLIC ADO Exam 2024

IBPS Clerk Exam 2024
My parents suggested me to join Veranda RACE and prepare for Bank Exams. Within 8 months, I've achieved a Bank job in Central Bank of India. I used to attend tests in the computer lab at my offline branch for more than 6 hours. My mentors cleared all my doubts and my faculty motivated me and taught focus strategies to clear the IBPS Clerk Exam.
Jebakumar
IBPS Clerk Exam 2024

SBI PO Exam 2024
Thanks to Veranda RACE, I've cracked three Bank Exams - IBPS PO, SBI PO and IBPS Clerk. Coming a village in Tuticorin, Veranda RACE faculty helped me understand the syllabus and topics of Bank Exams. With full focus on Bank exams, I used to prepare daily in the computer lab and library with constant support from my Bank mentors. They cleared all my doubts without any hesitation.
Thanga Vignesh
SBI PO Exam 2024

AIC MT Exam 2024
I prepared for Bank Exams in Veranda RACE’s Tambaram branch. They trained me specifically for the ‘Agriculture Insurance Company’ Exam. I’m happy that I could contribute more to the profession of my choice! Thanks to the faculty and mentors of Veranda RACE!
Amsalekha
Management Trainee, AIC

LIC ADO Exam 2024
Preparing from Tirunelveli, I want to thank my faculty for the constant support and motivation to crack the LIC ADO Exam. The lab facilities were top notch and I used to prepare writing online mock tests at the computer lab. This was the major reason for cracking the exam in the first attempt. Thanks, Veranda RACE!
Hariharasudhan
Junior Clerk-cum-TypistLIC ADO Exam 2024